Due to the COVID-19 pandemic, Medicaid programs were required to keep people enrolled through the end of the public health emergency. This might have helped millions of families avoid falling deeper into poverty, particularly those in communities of color, which were disproportionately affected by the pandemic.
However, this provision has ended, allowing states to restart Medicaid eligibility reviews and terminate coverage for those found ineligible – a process known as “Medicaid unwinding.”
Earlier this month, the Southern Poverty Law Center’s lobbying arm, the SPLC Action Fund, joined several civil rights and health care groups to release Six Months into Unwinding, a report examining the impact of this process.
Here are the top five takeaways from the report:
- Unwinding Medicaid has resulted in the largest two-year drop in Medicaid coverage in history – a net loss of at least 5.3 million people. This figure recognizes ongoing Medicaid enrollment. The gross number of terminations was 10 million people, and those losing coverage were likely uninsured at least for a brief period.
- Communities of color are overrepresented in the Medicaid population, accounting for 5.4 million people out of the 10 million gross losing coverage during the unwinding. These communities also face more barriers to accessing health care services and coverage. For example, they are less likely to have access to the internet, transportation and flexible job schedules.
- More than 70% of people losing Medicaid may lose it due to missing paperwork – not because they were found ineligible. People in this situation often received confusing notices or never received their renewals. Georgia, a state within the region served by the SPLC and SPLC Action Fund, was among the top 10 offending states with the highest rates of “procedural terminations.” States with lower paper termination rates made more investments in data collection and matching to automatically renew eligible people.
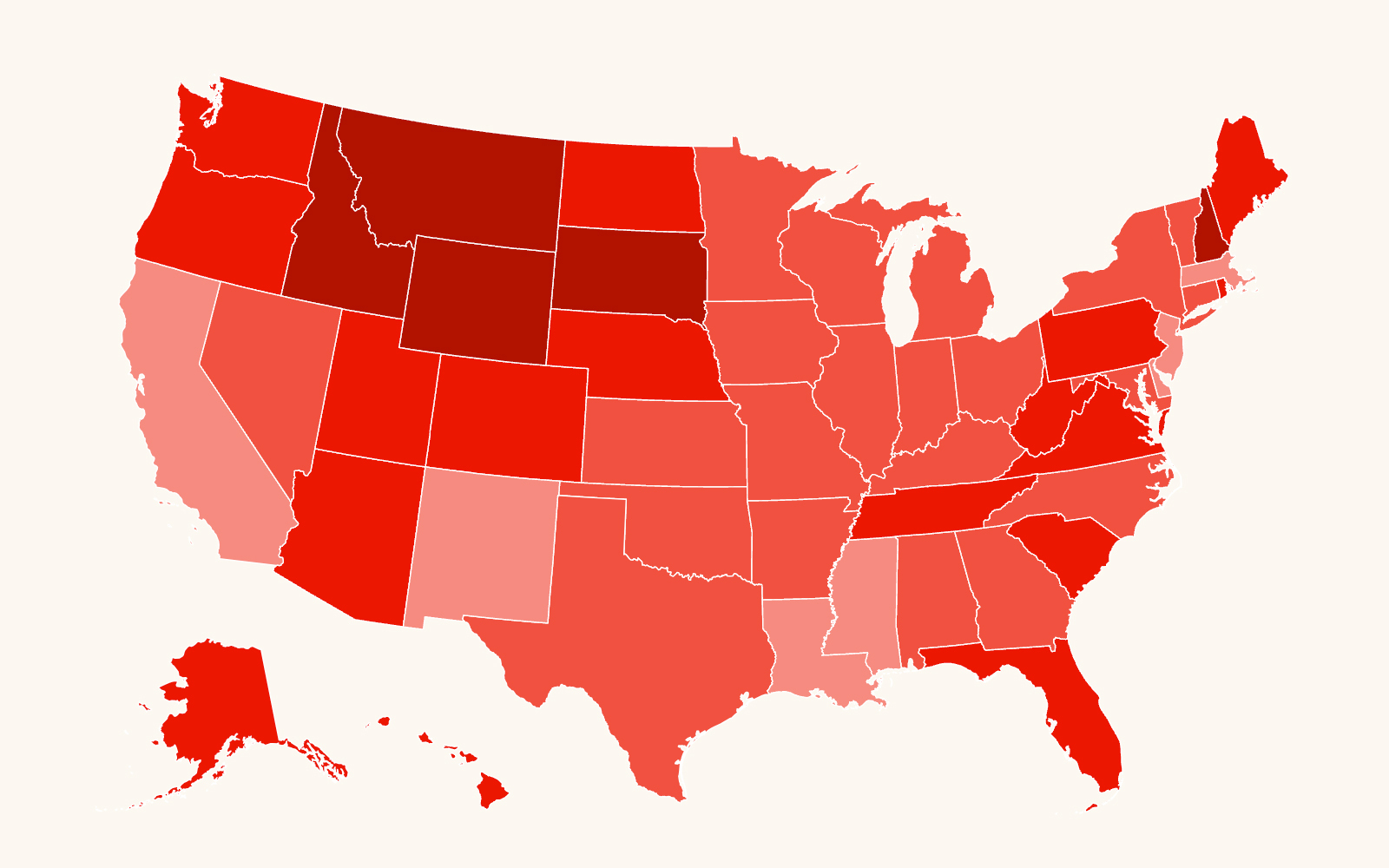
- The loss of Medicaid varies significantly by state. States that have not expanded Medicaid, such as our Deep South states, will be more severely impacted by the termination of health care coverage. That’s because more people will fall into the coverage gap where their incomes are above their state’s eligibility for Medicaid, but below the poverty rate for insurance subsidies through the Affordable Care Act marketplace. Residents from Alabama, Florida, Georgia and Mississippi make up over 40% of the adults in the coverage gap nationwide. People of color make up about 60% of the coverage gap nationwide.
- States should do more to reduce the massive numbers of people losing health care coverage. States need to stop the hemorrhaging of coverage by pausing terminations, making more investments in call centers and administrative support, and using more reliable data to automatically renew people.
The report results, while sobering, are not shocking. The recommendations are particularly salient to Deep South states where we are hearing stories of children being denied lifesaving care or families never getting their termination notices. We should demand that states stop terminations until their process is ensuring eligible people have coverage. We need to demand that states invest more in our health care systems. And we need to expand Medicaid coverage to ensure everyone has access to health care.
Theresa Lau is the SPLC and SPLC Action Fund senior policy counsel for eradicating poverty.
Illustration at top: Medicaid programs were required to keep people enrolled through the end of the COVID-19 pandemic, but that provision has ended. (SPLC)