Tina, a 58-year-old Black woman living in the Delta, is Mississippi born and raised.[1] She raised four children and spent more than two decades working as a machine operator at a catfish plant. While she has Medicaid coverage now, there was a time when she felt she could not see the doctor because she could not afford it. Before Medicaid, she would ration or depend on her community to help her keep up with her prescriptions.
“[There] was a time where I wasn’t able to go to the doctor, but I thank God for friends and my kids. That’s one thing — [since] they knew I didn’t have any insurance. One was going to make sure I had the fee for the doctor, one was going to pay for the meds, one was going to buy gas, and somebody was going to give me something to eat on. So, I thank God for that. My kids were my support system.”
— Tina
It took Tina six months to get her Medicaid application approved because of all the red tape in accessing the very program meant to help people with low incomes get health care. While Tina’s experience with Medicaid is unique, many people across the Deep South are in similar positions. Even still, Medicaid plays a critical role in ensuring people with low incomes — especially people of color — access health care they otherwise would not be able to afford.
Introduction
Annual wellness and school physicals. Monthly prescription refills. Urgent care sick visits. For many, these are routine matters made possible through access to quality health insurance. However, for far too many Black people across the Deep South, these health care benefits are out of reach due to inequities in our health care system — inequities that stem back to the very founding of our nation.
Indeed, the harsh living conditions, malnutrition, and other forms of torture enslaved Black people endured, coupled with their inability to access or afford health care, set the foundation for racial health disparities in this country for generations. This legacy of health care inaccessibility — and eventual poor health outcomes — is still profoundly felt by Black communities across the country. Today, Black women suffer from some of the highest levels of diabetes and high blood pressure in the country, Black men’s risk of a stroke is twice that of white men, and Black people are more than twice as likely to suffer from Alzheimer’s and other kinds of dementia compared to white people.
Importantly, the Deep South epitomizes these racial health disparities. For example, in 2023, Black Mississippians had the highest death rate from heart disease, high blood pressure, stroke and diabetes in the state — deaths that were all potentially preventable with proper medical treatment. Black Floridians were more likely to die from kidney disease compared to white Floridians. Indeed, with proper care, there could be many more people in the world to attend events with friends, many more to celebrate milestones with their loved ones, and fewer dining chairs left empty during family dinners. Clearly something must change at the systemic level to keep Black people from needlessly dying from treatable and preventable illnesses.
The good news is, our nation has already established a solution to redress these racial disparities: Medicaid.
Medicaid is a government health insurance program whose primary purpose is to provide health insurance to people with low incomes and disabled people. Nearly 50 million people rely on this critical program to help them see the doctor, visit the emergency room, and receive long-term care. In the Deep South (Alabama, Florida, Georgia, Louisiana and Mississippi) alone, there were almost 9 million people enrolled in Medicaid as of 2023. Access to Medicaid in the Deep South is a crucial lifeline because the region has one of the highest percentages of people living in poverty in the United States. Notably, Medicaid covers populations of people who are less likely to be able to afford or have access to private insurance — the very reason the program was created in the first place.
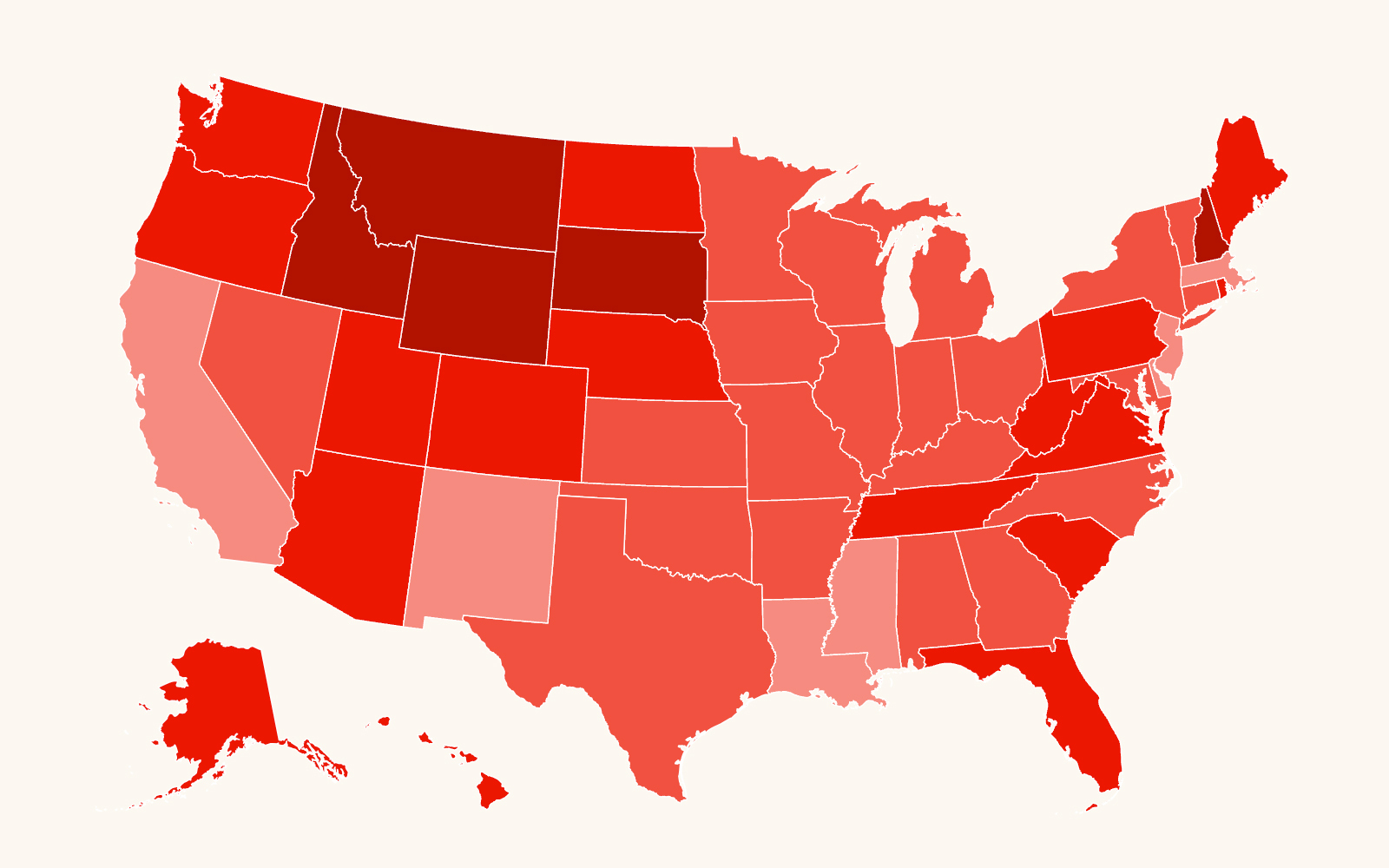
Medicaid is administered by states but is jointly funded by both state and federal funds. Medicaid as it currently operates, however, is in dire need of reform to fully combat the racial disparities in health outcomes and health care access present across the Deep South. States have great flexibility to decide how to run their Medicaid programs — including what populations of people to cover. Of note, prior to the Affordable Care Act (ACA), most adults ages 19-64 with low incomes were generally excluded from eligibility. Medicaid expansion has been critical to reducing racial health disparities: Between 2013 and 2022, the gap in uninsured rates shrank by 67% between white and Black adults under age 65 in Medicaid expansion states. Additionally, Medicaid plays a critical role in ensuring people with disabilities, children, and rural communities get health care coverage — contributing to health equity. Despite the evidence that expanding health care coverage is a good thing, not all states have expanded — leaving many in health insurance limbo. Following the ACA in 2010, states can take advantage of federal incentives to expand the populations covered by Medicaid — a process commonly referred to as Medicaid expansion. As of 2025, 40 states and the District of Columbia have expanded access to their Medicaid programs beyond the narrowed pre-2010 populations. Prior to expanding Medicaid, states traditionally only covered people with low incomes, but eligibility for children in families with low incomes, older adults, disabled people and pregnant people was limited. Medicaid expansion includes coverage — and eliminates categorical eligibility (basing eligibility off predetermined categories) — for people with incomes up to 138% of the federal poverty line (about $20,780 a year for an individual and $35,630 a year for a family of three).
However, as a continuing result of partisan stances, several states across the Deep South[2](including Alabama, Florida, Georgia and Mississippi) have failed to expand, leaving many in a “Medicaid coverage gap” — meaning they cannot afford private health insurance through companies, yet they do not qualify for Medicaid coverage in their state because their income is too high. Across Alabama, Florida, Georgia and Mississippi, there are over 1.1 million people who would become eligible for Medicaid if their states expanded. People living in the coverage gap are not a monolith, and expansion would help people across the board. In Deep South nonexpansion states like Florida, Georgia and Mississippi, more than half of the people in the coverage gap are people of color. This pattern is not unique to the Deep South. In fact, across the U.S., nearly half of people in the coverage gap are people of color.
Evidence continuously demonstrates that Medicaid is of vital importance to people and families across the country. However, the federal government has made numerous inroads to dismantle or severely limit federal funding for the Medicaid program, especially in the past couple of years. For example, the Trump administration made it a campaign promise to cut social safety net programs, and Medicaid cuts were a major part of the fiscal year 2025 budget reconciliation process. Regardless of the outcome of this year’s budget, states must step in to cover people in need of health care.
This report makes the case for Medicaid expansion in the Deep South as a pressing matter of racial and disability justice, centering on the voices of people directly impacted by health care inequities in the region. First, this report explores the history of racism in health care — highlighting how medical experimentation on Black people’s bodies laid the foundation for modern health care, yet Black people are overwhelmingly unable to access that very health care. Second, it examines the origins of Medicaid as public health insurance. This report also highlights the experiences of real people in the Deep South who are reliant on Medicaid to keep themselves and their families healthy. Additionally, this report will analyze the benefit Medicaid expansion would have in the Deep South for communities across the board.
The Southern Poverty Law Center uses people-first language, following guidance from reference sources such as the Associated Press Stylebook, the Publication Manual of the American Psychological Association, and the Reporter’s Guide from Street Sense Media suggesting that collective nouns such as “the poor” are dehumanizing.
Structural Racism in Early American Health Care
Inequitable health care access is embedded into the foundation of our nation, dating back to slavery. Enslaved people, subject to long and torturous work hours, did not have the agency to decide when to seek care for themselves and their families from a medical professional. In fact, many times medical care was only provided by enslavers as a last resort to protect their financial investment — not the enslaved person’s quality of life. After emancipation, Black people continued to have difficulty accessing health care; this barrier led to the creation of the Bureau for the Relief of Freedmen and Refugees, commonly known as the Freedmen’s Bureau. Established by the federal government, the bureau offered a range of support and resources that included emergency and temporary health care until states could assume permanent responsibility for their newfound citizens. This was one of the first documented efforts in the nation where the government attempted to redress some of the harm caused by structural inequity, such as health care disparities. However, factors such as limited funding, racism against formerly enslaved Black people, and mounting political pressure from Southern states forced the bureau to close in 1872 — just a few years after it was formed.
There Would Be No Modern Health Care Without Southern Black People
Today’s modern health care system would not be possible without Southern Black people, even as the same people have been summarily divorced from accessing it. Against their will, Southern Black people have often historically been forced to participate in medical experimentation. While these experiments were used to advance the medical field, with many of the physicians who participated in these practices celebrated for their contributions, many of the Black people who made these discoveries possible have been nearly erased from history.
One example of this is the abuse of enslaved Black women in Alabama to advance modern gynecological procedures in the 1840s by the “father of American gynecology,” J. Marion Sims. Sims experimented on women who were enslaved without the use of anesthesia, with some of these women being subjected to more than 30 surgeries while he tried to perfect his surgical technique. Sims was credited with discovering a cure to a gynecological ailment and was the first United States physician to have a statue built in his honor, while these enslaved women were largely erased from this shameful history. As part of an effort to reshape and retell this history from the perspective of the women and girls who were impacted, a monument honoring the Mothers of Gynecology was completed in Montgomery, Alabama, in 2021 — the first memorial to ever list their names.
Another example, the “Tuskegee Study of Untreated Syphilis in the Negro Male,” was a 30-year-plus study of at least 600 African American men from Macon County, Alabama. In 1932, the U.S. Public Health Service began an experiment to observe the natural course of untreated syphilis without medical intervention, with participants largely consisting of sharecroppers living in the “Black Belt” of Alabama. The participants in the study were not given accurate information about their diagnosis as they were told they were going to be treated for “bad blood,” a vague term used to describe illnesses ranging from anemia to fatigue. Participants were lied to about the study’s purpose, their medications, and their treatment plans — and thus could not give informed consent to be tested on in the first place.
By the end of this study that spanned many decades, dozens of men, their wives, children, and others had been infected with syphilis. A class action suit was filed on behalf of those who were impacted by the study, and a settlement of more than $9 million was given to the study participants. On May 16, 1994, an apology at a White House ceremony was finally made to the surviving participants of the study and families of those who had died.
The Tuskegee study, as well as J. Marion Sims’ forced medical experimentation on women who were enslaved, are just two examples among many of Southern Black people being used — at times, without their consent — to advance modern medicine.
However, the cruel irony is that even in present day, Black people have less access to the health care and treatment that modern medicine offers. This underscores the urgent need for policymakers to create reparatory policy solutions that begin to rectify the medical harm Black people have experienced throughout history.
The Creation of Medicare and Medicaid
Before 1965, people who could not afford private insurance were dependent on states, localities or charities to provide health care access. During this same period, the use of health and hospital services also varied by race, as did the level of care segregated hospitals provided. In recognition of these disparities, President Lyndon B. Johnson signed two national health care programs — Medicare and Medicaid — into law in July 1965 to help equalize access to health care. After its creation, the Medicare program primarily covered people over age 65. At the same time, the Medicaid program provided coverage for certain people and families with low incomes. Both Medicare and Medicaid started as basic insurance programs for people who did not have health insurance. Both programs have evolved over time to include coverage for more medical services and groups of people — including children, parents, pregnant people, seniors, and people with disabilities — who otherwise would not be able to access health coverage.
Medicaid as a Lifeline Across the Deep South
“At the end of the day, the [Medicaid program] should be to help people who need it, and not to judge if or why they really need [assistance].”
— “Anonymous”
Since its implementation, Medicaid has served as a critical source of health care coverage for many vulnerable communities, including people of color, people with disabilities, and members of the LGBTQ+ community. For example, after Medicaid’s enactment, access to health care expanded for Black people, with 1 in 5 Medicaid enrollees across the country being Black as of 2022.[3] The top five counties with the highest number of Medicaid recipients in each Deep South state also have a high percentage of Black people living in the county. (See graphics that follow.)
Alabama
In Alabama, there were 1,310,256 Black people living in the state between 2018-2022 (five-year estimate).
Florida
In Florida, there were 3,248,401 Black people living in the state between 2018-2022 (five-year estimate).
Georgia
In Georgia, there were 3,350,394 Black people living in the state between 2018-2022 (five-year estimate).
Louisiana
In Louisiana [4], 1,392,840 people received Medicaid between 2018-2022 (five-year estimate).
Mississippi
In Mississippi, there were 1,088,106 Black people living in the state between 2018-2022 (five-year estimate).
Deservingness, Government Aid and Poverty
In the United States, anti-Black racism and sexism have permeated the public’s perception of people experiencing poverty — with poverty treated as a personal failure rather than a product of intentional policy choices that have created an inadequate system of supporting people during financial crises. In the 1980s, President Reagan supported cutting public aid programs by repeating the “welfare queen” trope, which pushed the false narrative that Black women especially will abuse cash aid. During his second inaugural address, President Reagan claimed he wanted to help families experiencing poverty “escape the spider’s web of dependency.” The very support systems purported to help people with low incomes suppress wealth-building opportunities by prioritizing connection to short-term employment rather than education and training — continuing the lengthy history of limiting access to support meant to reach people who need it most to control Black people. The idea that poverty is a personal failure is primarily rooted in false, racist tropes of Black people like “the welfare queen” — the stereotype that Black women experiencing poverty who receive cash assistance from the government will continue to have more children to keep receiving help from the government rather than earning their own income. In addition to impacting cash assistance, these stereotypes have also permeated the policy decisions made in Medicaid’s operation. For example, eligibility for Medicaid was once linked to the receipt of Aid to Families with Dependent Children (AFDC), a cash assistance program for families with dependent children under age 18 experiencing poverty. In other words, families were automatically able to get Medicaid coverage if they were receiving AFDC cash assistance. In 1996, however, AFDC was replaced by the Temporary Assistance for Needy Families (TANF) program, and the link between cash assistance and Medicaid eligibility was no longer automatic. This decision created a hurdle to health care for people who would have qualified in the past, thereby limiting coverage for people who otherwise could not afford it. Fueled by racist stereotypes about Black people’s overreliance on government assistance programs, this decision was yet another attempt to weaken safety net programs, making benefits more difficult to access.
States Perpetuate Racial Inequities in Medicaid Coverage
States have a large say in how their programs are conducted in part because of the Affordable Care Act (ACA). Under the Obama administration, the ACA was enacted in 2010, and it expanded eligibility for Medicaid by incentivizing states with the promise of increased federal funding to run their programs. Prior to the ACA, Medicaid only covered specified categories of people with low incomes: pregnant people, children, parents of dependent children, people with disabilities, and people aged 65 and older. States were required to cover individuals in these groups up to federal minimum income thresholds, but they also had the option to expand coverage to people at higher income levels if they wanted to.
Importantly, prior to the ACA, adults ages 19-64 with low incomes were largely excluded from Medicaid. The ACA attempted to require that all states cover nearly all people who had incomes at or below 138% of the federal poverty level ($15,415 per year for an individual in 2012). This included people under age 65, who were not pregnant, ineligible for Medicare, and were not described in an existing mandatory coverage group — also known as “Medicaid expansion under the Obama administration.” However, this Medicaid expansion requirement and other parts of the ACA were quickly challenged in the courts as a federal overreach, in the National Federation of Independent Business v. Sebelius case.[5]
In short, after Sebelius, the court effectively made Medicaid expansion a state-by-state option by holding that requiring states to expand under threat of losing their federal funding was outside of congressional authority. Although not mandatory, a state is incentivized to expand because the amount of federal matching dollars for its Medicaid program increases to cover additional people in those mandatory coverage groups.
As of 2024, 40 states and the District of Columbia have adopted Medicaid expansion, including Louisiana in the Deep South. However, there are still 10 states that have not adopted expansion, and at least four of those states are in the Deep South — Alabama, Florida, Georgia and Mississippi — despite increasing interest and recent legislative efforts to expand in some of these states. For example, HB 1725, which attempted to expand Medicaid, passed the Mississippi House of Representatives by an overwhelming 99-20 vote in 2024 — even though the bill failed in the Senate.
Medicaid and COVID-19
During the COVID-19 pandemic, the American Rescue Plan Act (ARPA) offered emergency assistance funding and required that states kept people enrolled through the end of the public health emergency. This provision helped many people qualify for Medicaid who would ordinarily be ineligible in nonexpansion states. Following the end of the pandemic-era assistance, states started conducting eligibility reviews and terminating health care coverage for those who were previously covered before the review — a process known as “unwinding.” The Southern Poverty Law Center’s report, Six Months into Unwinding: History’s Deepest Medicaid Losses Demand State Action, provides more information on how Medicaid assistance during the pandemic helped millions avoid falling deeper into poverty, and how unwinding negatively impacts people of color — especially Black people, families and communities.
Case Studies
The Case for Preserving Current Medicaid Coverage Expansion
“We need to have more options. We need to have people that come out and listen to us when we in the doctor’s office and listen to our [experiences] … They need to get out here and see firsthand what’s going on in the doctor’s office, because it’s a lot of [budget] cuts and a lot of times we don’t know what has been cut, what has been taken out, and most of the time if it’s something added in, it’s not benefiting us.”
— Tina
While we cannot change the policy choices made in the past, there is hope and a way forward — one that involves preserving current Medicaid coverage and expanding Medicaid for the states that have yet to do so, especially the states in the Deep South. There are several benefits to Medicaid expansion, such as increased access to health care for people of color and people with disabilities, the preservation of rural community hospitals, and ensuring marginalized communities have access to the basic health resources they need.
Further, investing in Medicaid expansion can generate significant economic activity for states too. Research finds that Medicaid expansion results in increased revenue as well as net savings due to decreased state spending on catastrophic care. In Louisiana, Medicaid expansion created 19,000 jobs and generated more than $3.5 billion in economic activity in the state.
For these reasons and more, the SPLC recommends that all states across the Deep South preserve current Medicaid coverage and expand Medicaid to more families in need by doing the following:
- Reject proposals that reduce state and federal money going towards Medicaid. Cutting funding for Medicaid will ultimately impact people experiencing poverty and their ability to receive potentially lifesaving health care. Additionally, the reduction of funds impacts care providers who depend on funds to be able to offer care to vulnerable communities.
- Expand Medicaid to include coverage for adults with low incomes at least up to 138% of the federal poverty level without added work requirements. Expansion would shrink the coverage gap and offer health care coverage and access to people ages 19 to 64, many of whom are more likely to have disabilities and work jobs that have no path to employer-sponsored coverage.
- Bundle Medicaid assistance with housing assistance to help people with low incomes who have disabilities get back on their feet. All people need access to health care and housing. States can seek waivers such as a Section 1115 demonstration from the Centers for Medicare and Medicaid Services to explore the impact of covering housing-related services to people experiencing homelessness under Medicaid. Some states like Arizona are already taking advantage of this opportunity with programs that focus on providing stable housing and health care to people with mental illness and chronic health conditions.
Illustration by Xinyue Chen.
Acknowledgments
The Southern Poverty Law Center would like to thank the organization’s Georgia and Mississippi policy teams, the Mississippi state office, Andrea McChristian, and Delvin Davis, interim policy research director, for their support in guiding and reviewing this report. Thank you also to “Anonymous” in Georgia and Tina in Mississippi for their contributions to the report.
Policy
Gina Azito Thompson,
Policy Analyst
Eradicating Poverty
Editorial
Brad Bennett,
Editorial Director
Creative
Chris Mihal,
Creative Director
This report includes hyperlinked citations instead of full endnote citations. Full endnote citations, however, are available here.
[1] Video interview with Tina Payne conducted by Myisa Plancq-Graham, April 28, 2025, Leland, Mississippi.
[2] While included in the Deep South, Louisiana adopted Medicaid expansion in 2016. For more information regarding Medicaid expansion in Louisiana, see Kavita Patel, “From Worst to First: Louisiana Makes Great Waves with Medicaid Expansion,” Brookings Institution, January 15, 2016, https://www.brookings.edu/articles/from-worst-to-first-louisiana-makes-great-waves-with-medicaid-expansion/.
[3] Estimates based on the 2008-2023 American Community Survey, 1-Year Estimates.
[4] Louisiana adopted the Medicaid expansion in 2016.
[5] Of note, in the National Federation of Independent Business v. Sebelius case, the issue of Medicaid expansion as well as the individual mandate were challenged.